Spinal Cord Stimulation In Severe Intractable Painful Diabetic Neuropathy :
Diabetic neuropathy is defined as the presence of symptoms and/or signs of peripheral nerve dysfunction in people with diabetes after the exclusion of other causes Neuropathy is the greatest source of morbidity associated with diabetes, affecting up to 50% of those with long-standing disease, and pain as a symptom of neuropathy may be seen in as many as one third of all patients with diabetes.In the past, a lack of awareness and inappropriate management of diabetic peripheral neuropathy (DPN) has led to much unnecessary morbidity and substantial health care costs. At least half of all foot ulcers, the end stage, should be preventable by appropriate management and patient education.
Approximately 50% of patients who have had diabetes for more than 25 years will develop neuropathy. Approximately 50% will have pain as a symptom. Neuropathy is usually a late finding in type 1 diabetes; however, it can be an early finding in type 2 diabetes.Hyperglycemia (high blood sugar) is highly correlated with the development and progression of all neuropathies. The Diabetes Control and Complications Trial (DCCT) showed that tight glycemic control will reduce the incidence of neuropathy by 60%. However, even in patients with long-term excellent glycemic control (HbA1C < 8%), the lifetime incidence of Diabetic peripheral neuropathy (DPN) remains 20%.
Some people have mild symptoms. But for others, diabetic neuropathy can be quite painful and disabling.Diabetic neuropathy usually affects the feet and legs first, followed by the hands and arms. Signs and symptoms of peripheral neuropathy are often worse at night, and may include:
- Numbness or reduced ability to feel pain or temperature changes
- Tingling or burning sensation
- Sharp pains or cramps
- Increased sensitivity to touch — for some people, even a bedsheet's weight can be painful
- Serious foot problems, such as ulcers, infections, and bone and joint pain.
Diabetic neuropathy is usually diagnosed by carefully reviewing your symptoms and medical history and then performing a physical exam.Clinical examination including Overall muscle strength and tone, Tendon reflexes and sensitivity to touch and vibration is done Along with the physical exam, specific tests help diagnose diabetic neuropathy, such as:
- Filament test. A soft nylon fiber (monofilament) is touched over areas of your skin to test your sensitivity to touch Sensory testing.This noninvasive test is used to tell how your nerves respond to vibration and changes in temperature.
- Nerve conduction testing.This test measures how quickly the nerves in your arms and legs conduct electrical signals. It's often used to diagnose carpal tunnel syndrome.
- Muscle response Called electromyography, this test is often done with nerve conduction studies. It measures electrical discharges produced in your muscles.
- Autonomic testing. Special tests may be done to determine how your blood pressure changes while you are in different positions, and whether you sweat normally.
- The physical exam should also evaluate for signs of decreased arterial flow, altered reflexes, deformities, ulcers, or slow-healing wounds.
- Arterial flow is assessed using Doppler ultrasound
Treatment has three main goals including slowing progression of the disease, managing pain and managing other complications. Slowing progression of the disease is very important. This is done by controlling blood sugars very well. The diabetologist will be the best person for this. If however the pain has set in and very severe we need to treat it.
Managing pain is the need for most patients. The pain occurs in most patients due to reduction in blood supply to the nerves. Diabetes causes microangiopathy that is it affects the small blood vessels of the body. This causes severe pain in the legs which is called the cry of the dying nerves. If this is not treated over time the ain disappears because the nerves are dead. Then slowly the blood vessels get affected resulting in amputation
The treatment of this pain also can be through the WHO analgesic ladder. For localised pain (for example, dorsum of foot) Capsaicin cream (0.075%) applied four times/day (maximum 6–8 weeks) can be useful. For generalised pain drugs like gabapentin/pregabalin along with duloxitene/amitryptline are good. Other similar alternatives include newer drugs like a- lipoic acid (ALA), ?linolinic acid (GLA), Isosorbidedinitrate spray, acupuncture etc. All of them only give symptomatic relief but do not but they do not take away the reduced blood supply
About 60 to 80% of patients in the initial stages do benefit from all these conservative measures. But some patients either do not get any benefit from these methods or develop severe side effects due to the drugs. Such patients can be offered neuromodulation procedures
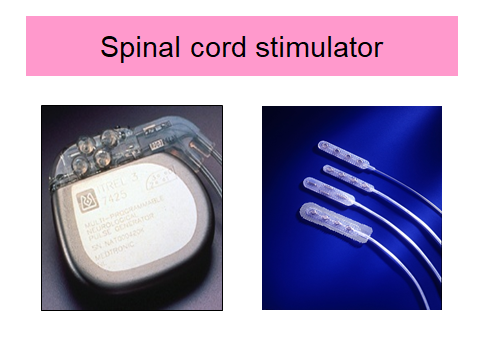
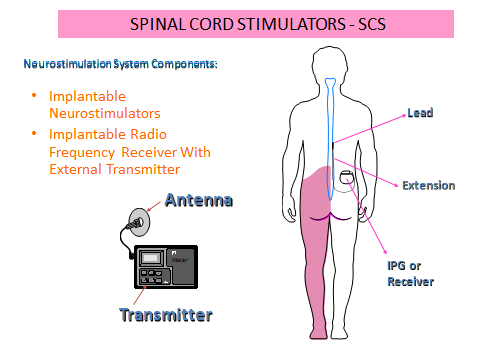
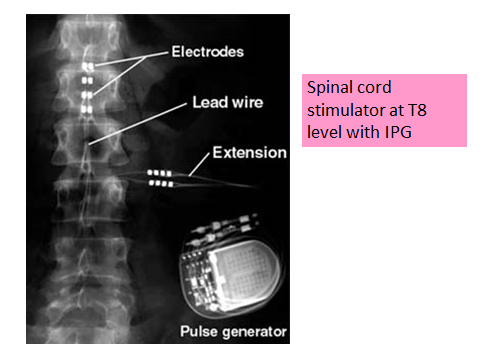
The best neuromodulation technique for diabetic neuropathy pain is Spinal Cord Stimulation (SCS). This delivers electrical stimulation to the dorsal column (back portion) of the spinal cord through implanted electrode and is connected to an electrical stimulating device usually placed in the lower abdomen. SCS is usually reserved for treatment of pain in patients with neuropathic pain who have not responded to conventional treatment. Up to 70% of these patients have reported pain relief one year after initiating treatment with SCS.Many studies have shown the good outcome with SCS.Spinal cord stimulation (SCS) involves an electrical generator that delivers pulses to a targeted spinal cord area. Leads are implanted by laminectomy/percutaneously. The source of power is an implanted battery or external radio-frequency transmitter. The exact mechanism of action of SCS is poorly understood.
Results of SCS are very good with long studies showing good pain relief even at 5 years after implantation. It has also been shown to have very good long term cost effectiveness. The surgery is very simple and patients can go home with 24 hours of surgery. Some studies have even shown that requirement of insulin can be reduced after spinal cord stimulation.